Maryland Eliminates Trans Healthcare Exclusions
Policy change will allow insurance to cover transition-related health care costs
FreeState Legal, the legal advocacy organization working on behalf of low-income LGBTQ Marylanders, announced Tuesday that the state of Maryland, in response to the threat of a lawsuit, has changed its employee health care policy to provide insurance coverage for medically necessary care for transgender state employees.
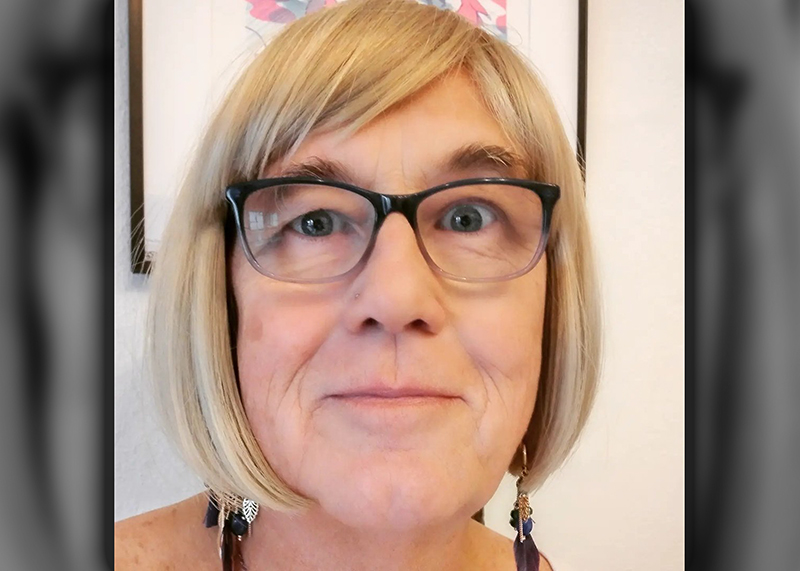
FreeState Legal filed its first claim against the state in November 2013 on behalf of Sailor Holobaugh, a transgender man employed by the University of Maryland at Baltimore, who was denied coverage for a medically necessary bilateral mastectomy, on the basis of a provision that, heretofore, had exluded coverage for any “procedure or treatment designed to alter an individual’s physical characteristics to those of the opposite sex.” FreeState Legal argued that the state’s denial of coverage to Holobaugh violated Gov. Martin O’Malley’s 2007 executive order prohibiting discrimination on the basis of gender identity in state employment. In January, the organization filed an additional discrimination complaint with the Maryland Commission on Civil Rights.
As part of the settlement for both claims, reached outside of court, the state has removed all language that denies coverage to transgender people for medically necessary transition-related health care expenses, and has instituted a new comprehensive “gender dysphoria benefit.” The state has also reimbursed Holobaugh for his out-of-pocket costs for his surgery.
The gender dysphoria benefit provides coverage for medically necessary transition-related care, including hormone replacement therapy and certain surgical procedures. The standard established for what constitutes medically necessary care closely tracks the “Standards of Care” issued by the World Professional Association for Transgender Health (WPATH), the leading international authority on health care for transgender people.
The benefit is effective immediately, and applies to all participants in the State Employee & Retiree Health & Welfare Benefits Programs, including the spouses and dependents of current employees or retirees.
“Maryland has moved one step closer to achieving full equality and justice for transgender Marylanders, Aaron Merki, the executive director of FreeState Legal said in a statement. “We applaud this development, and look forward to a time when these discriminatory exclusions are removed from all public and private health insurance policies.”
“My experience as a social worker and a Scout has made me appreciate the importance of persevering for change and equality,” Holobaugh said in a statement. “I am thrilled that people who serve Maryland as state employees now have increased access to health services, and that they can extend these benefits to their dependents.”
The policy change makes Maryland the fourth state in the nation to provide nondiscriminatory health coverage to transgender state employees, according to the National Center for Transgender Equality (NCTE).
“We applaud Maryland and the administration of Governor O’Malley for becoming the fourth state to ensure coverage of transition-related care for state employees, joining Massachusetts, Oregon and California, along with the District of Columbia,” Mara Keisling, the executive director of NCTE, said in a statement.
In an additional statement, FreeState Legal also vowed to continue to fight any remaining exclusions within Maryland’s laws, specifically focusing on private insurance regulated by the Maryland Insurance Administration, self-funded employee health benefit plans, and the state’s Medicaid program.
“With the passage this year of the Fairness for All Marylanders Act and the establishment of the state employee Gender Dysphoria Benefit, Maryland is making great strides toward transgender equality,” Jer Welter, the managing attorney of FreeState Legal who represented Holobaugh, said.
“However,” Welter continued, “there is still work to be done, including the elimination of similar transition-related care exclusions in the Maryland Medical Assistance (Medicaid) program and in polices issued by private insurers regulated by the Maryland Insurance Administration. FreeState Legal will continue to work diligently on these issues to further ensure that equal and fair health coverage is a staple for all LGBTQ Marylanders.”
A spokesman for NCTE told Metro Weekly that six states – California, Colorado, Connecticut, Massachusetts, Oregon and Washington State – and the District of Columbia mandate coverage of transition-related care in private insurance. In addition, California, Massachusetts and the District of Columbia also have provisions in place that explicitly cover transition-related care in their Medicaid programs.
Support Metro Weekly’s Journalism
These are challenging times for news organizations. And yet it’s crucial we stay active and provide vital resources and information to both our local readers and the world. So won’t you please take a moment and consider supporting Metro Weekly with a membership? For as little as $5 a month, you can help ensure Metro Weekly magazine and MetroWeekly.com remain free, viable resources as we provide the best, most diverse, culturally-resonant LGBTQ coverage in both the D.C. region and around the world. Memberships come with exclusive perks and discounts, your own personal digital delivery of each week’s magazine (and an archive), access to our Member's Lounge when it launches this fall, and exclusive members-only items like Metro Weekly Membership Mugs and Tote Bags! Check out all our membership levels here and please join us today!



























You must be logged in to post a comment.