The CDC’s Demetre Daskalakis on Containing the Spread of Monkeypox
The Deputy Coordinator of the White House monkeypox response breaks down the CDC's strategy to control the outbreak.

As the global HIV/AIDS science and public health community convened in Montréal last week for the International AIDS Society’s AIDS 2022 conference, a different infectious disease emerged as the hot topic among the thousands of delegates and media in attendance, and it wasn’t COVID.
Monkeypox was discussed with urgency and professional enthusiasm throughout the bustling conference — in packed sessions, in passing, over post-session dinners in charming Old Port restaurants.
Accordingly, IAS organized both a prime-session symposium on the current multi-country monkeypox outbreak and response, as well as an informal media roundtable, where officials from the WHO and U.S. CDC, among other experts, provided the press an on-the-ground update on this latest global health emergency.
Just prior to the conference, WHO Director-General Dr. Tedros Adhanom Ghebreyesus had declared the monkeypox outbreak a public health emergency of international concern (PHEIC). WHO statistics currently count over 26,500 lab-confirmed cases worldwide, in nearly 90 member-states.
Speaking at the media roundtable, Dr. Meg Doherty, WHO Director of Global HIV, Hepatitis, and STI Programs, explained that the emergency declaration “was based on the fact that [the outbreak] reached the three criteria of a PHEIC, which is it’s an extraordinary event, it is a public health risk to other member states, and it needs a coordinated response.”
The WHO has taken a strong stance to address the outbreak, said Doherty, adding that the organization’s “focus is very much on an equitable approach” to ensure that tools like testing and treatment are available everywhere they’re needed. They’re also committed, she said, to maximizing outreach to those at greatest risk of exposure to the disease.
“Our department has been working really closely with communities of MSM, and have had several other meetings that have brought MSM together to guide what kind of tools and language come out,” Doherty explained.
“We have been working as well with Facebook and a lot of social media groups, so that we can not only have a view on information that’s out there, [but] also be aware of disinformation and how we can combat and address some of that information that’s coming out as well. Certainly, we want to make sure that we don’t make the mistakes that we made with HIV, and that we’re also learning from not only HIV but learning from the COVID response.”
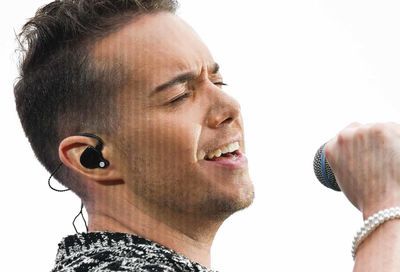
Dr. Demetre Daskalakis, Director, CDC Division of HIV prevention, presented at both monkeypox sessions at the conference, and similarly addressed the need to combat stigma associated with the disease. In June, as part of the CDC’s Monkeypox Response Team, he published an article in the Annals of Internal Medicine that addressed the issue specifically.
In Monkeypox: Avoiding the Mistakes of Past Infectious Disease, Daskalakis and his co-authors warned “[e]xperience has shown the dangers of characterizing a disease by associating it with a single population or a particular identity. Such associations can create stigma that outlives the outbreak and lost opportunities to detect and address the infection in other populations. Knowledge is power.”
On August 2, as the AIDS 2022 conference wrapped, President Biden named Daskalakis the White House National Monkeypox Response Deputy Coordinator, serving with FEMA’s Robert Denton, who was named White House National Monkeypox Response Coordinator.
Prior to stepping into his White House role — and days before Biden declared monkeypox a national health emergency — Daskalakis sat down with Metro Weekly at AIDS 2022 to discuss the CDC’s ongoing response to this fast-moving outbreak.
METRO WEEKLY: Something that came up in that roundtable session, is the fact that when these infectious disease outbreaks emerge, it generally falls to HIV researchers to be the first line of defense. Why is that?
DEMETRE DASKALAKIS: So, I think that the HIV infrastructure has been so important for so many infectious disease responses. And, you know, HIV is an outbreak, and it’s an outbreak that’s been going on for 41 years. And so people who have been working in HIV have been working in an emergency for four decades. So it is, I think, natural to look toward those leaders and scientists to sort of anchor the work, to be able to address new challenges, especially with monkeypox, specifically, given the overlap in the population, where it’s not only about the science and the response.
I’m going to say a statement for everybody, which usually you can’t do, but I think I’m comfortable saying that those of us who have done HIV work for decades feel a great responsibility to make sure that the missteps that happened at the beginning of HIV don’t happen at the beginning of monkeypox.
And I want to qualify that and say one moment of stigma can last decades. It’s a lesson that you learned from HIV that the stain of “gay-related immunodeficiency” is in our cultural DNA. Those of us who do HIV, who sort of lived through that or lived near it, or are from the experience of being a gay man, we are the watchdogs to make sure that that doesn’t happen again.
MW: You talked in the session about the pillars of the CDC strategy on monkeypox — testing, treatment, vaccines, and messaging, which gets into how some people already are interpreting monkeypox as a gay sexually-transmitted disease.
And particularly, as we see non-MSM having the disease, I’ve actually seen people on social media questioning, “Well, how does a child get a gay sexually transmitted disease?” So can you break down specifically what is the CDC messaging about? And is there any part of it that is directed towards anti-stigma?
DASKALAKIS: I’ll start by saying that the strategy, which is based on the hard lessons learned from HIV, is to make sure that we create information that is general and science-based, even with imperfect science. So we’ll start with that. And the second part — and this is a lesson from HIV and from COVID, as well as other outbreaks — is to make sure that you use trusted messengers, trusted platforms, and trusted networks to get the message out to the people who need to hear it the most, because of where the disease activity is happening.
So that is one stigma strategy, which is not to back off from talking to gay, bisexual, and other men who have sex with men, but also making the messaging evergreen and focused on everyone, also making sure that through the right networks, it’s getting to the people who need to know about it the most, which right now are gay, bisexual, and other men who have sex with men.
Very early on, we put out recommendations for how to communicate without generating stigma, because I think we know from public health responses that stigma, aside from being hurtful, also creates assumptions about diseases that aren’t true epidemiologically and then result in populations suffering.
And not just from the stigma, but actually also from the infection. So we’ve been really deliberate to make sure that we, through our own messaging and our guidance about messaging, centered stigma and equity from the very beginning. That’s been our path.
I can’t speak for what happened in 1981. I wasn’t there. I was still a little bit too young. But I don’t know if at that moment there was the same intentionality to say, “We’re starting in a place where we’re going to address stigma from the beginning, before we accidentally create it in our public health messaging.”
So, from my perspective as someone who’s been doing HIV for decades, it was inspiring to see a big public health organization like the CDC start with “Let’s not generate stigma, but let’s make sure that we’re telling people what they need to know.”
MW: This week, for example, we had the W.H.O. Director-General saying, basically, “Stay out of bathhouses — slow down, gay and bi men!” Contrast that with Fauci leading with “We really need to make sure that we’re not stigmatizing these people.” I think people out here are getting mixed messages. Who’s making an effort to create a unified message, so we’re all on the same page?
DASKALAKIS: No one’s disagreeing. I mean, [CDC’s] social gatherings and safer sex guidance, I think, is a really great example. The goal of that is to use our best knowledge — scientific and epidemiologic — to give people a range of what is harm reduction to really maximize their personal health. For some people who aren’t going to make a lot of changes — like what’s the minimum change that you can do to improve your outcomes? — to the people who will listen to every word you say and will absolutely, completely change [their] behavior while waiting for the biological intervention to be more robust. That’s been our strategy, and I think that we’ve been really, really frank.
For example, if you look at that guidance, we see that multiple and anonymous partners are associated with a higher risk of monkeypox exposure. So we say consider limiting your number of partners and your anonymous partners. And we also say, you know, there’s places where multiple and anonymous partnerships can happen. And we listed them, including bathhouses, sex clubs, private sex parties, etc. So people have the awareness that those are maybe venues that you may want to avoid.
I also think we’re enhancing our language around this to really make it clear that especially when we have a scarcity model with our vaccine, that these end up being really critical harm reduction strategies that are needed to help prevent monkeypox.
But the reality is — I’m not telling you anything you don’t know — the group, of gay, bisexual, or men who have sex with men are not a monolith. There’s so many different kinds of humans that live in that spectrum. And there are people who are at their baseline not particularly adventurous with their sex lives. There are people who are in the middle who can be adventurous sometimes, but not always. And there’s people who are always adventurous.
The goal is to shift everyone to a place where it is — with their awareness of how monkeypox transmits — within their context what makes the most sense so they can keep themselves healthy, and by extension, keep the community healthy. That’s really what we’re about. I don’t think that we have any daylight between us and the director-general. I think it’s just the wordsmithing. But I think it’s the same. When we say “consider avoiding multiple or anonymous partners,” we’re not really saying anything different than what he said.
MW: No, there is a difference in the tone, but the tone…
DASKALAKIS: Matters.
MW: It will affect how people behave.
DASKALAKIS: Yeah. And we know from HIV. This is not like me with a scientific public health hat, but me from the perspective of someone that’s done gay health work for a very long time. Whenever you say, “The only way to do this is X,” it never works. You end up alienating people because you’re, in effect, saying that what you’re doing is wrong.
So, what we can do is have folks nuance what their behavior and experience is to better align to what we know from the science in public health. And that’s the best that we can wish for. But I do think that people also look to public health for clear messaging. And so we try to update and nuance as we go along.
I think you’re going to see stronger messages from us that are going to say “consider avoiding.” I mean, we say it already, but we’re going to say it more. I’ve been saying it in interviews for weeks. But it’s really like you have to take that moment and say, “this isn’t like HIV.” If you are using a reduce-this behavior or reduce-that behavior, you’ll have to do it for a generation to be able to address HIV transmission. Monkeypox moves fast, which is a bad thing, but also a good thing. So if we are able to shift folks into a more harm reduction strategy, and reduce some of the opportunities for transmission while we’re increasing vaccine, we can get the outbreak under control faster.
MW: Speaking of getting it under control, Dr. Marina Klein, from McGill University in Montréal, said that they are seeing evidence of cases plateauing there. In the U.S., is it only going in one direction?
DASKALAKIS: It’s going up. I do not doubt that there’s going to be impact from the work that they’re doing [in Montréal]. The multifaceted work, like not only the vaccine, but also the prevention work that they’re doing, and the messaging — because they’ve been really good in Montréal, and in Canada, as well, at messaging. But I’ll also say you have to be really cautious with plateaus. So there are other countries that showed plateaus, and then it changes. There’s a lag. There’s also some testing issues that happen across the world. So I hope their plateau is real. I believe that they’ve done fabulous work. But I would tend to be hesitant until I see that the curve is going down.
MW: What does the CDC know about those who have tested positive for monkeypox who are not men having sex with men? What do we know about their exposure, or how mild or severe their symptoms have been?
DASKALAKIS: I can’t speak to it in a lot of detail. But definitely we’re hearing about, some of the exposures are related to close contact and sexual contact. I think a range of behaviors are happening among non-men who have sex with men. With that said, the vast majority — like the vast, vast majority are men who have sex with men.
As we see more of the outbreak, we’re going to be able to define it better. But at this stage, there’s nothing I can define as a trend. There’s no trend.
MW: What role will the CDC play in the distribution strategies for monkeypox vaccine? I realize that the states are allotted what they get. I was just reading about Maryland, for example, which initially received 3,363 doses of vaccine, 200 of which went to Baltimore, 200 to Montgomery County, and 200 to Prince George’s County, which seems extremely paltry, especially for Baltimore City. After a state has made these decisions, does the CDC have any further role in helping define how they distribute vaccines?
DASKALAKIS: So it’s important to say that we help, we sort of define the allocation of what the state gets, and then we provide them the technical assistance and other guidance and try to optimize their distribution.
What they ultimately choose to do for their distribution is in their wheelhouse. It’s their choice. But we definitely give them guidance, especially around equity. If you’re going to be doing things like first-come, first-serve strategies, which is what’s going on, there are still ways to make them more equitable.
I’ll give an example. I volunteered to give vaccines locally in Atlanta. I went to two vaccine efforts. And one of them, they just did a first-come, first-serve. And it was a very, not necessarily diverse population coming. The second one, they did small equity interventions, like helping community organizations to help people sign up, giving a little bit of a leg up to people who are in Black and brown communities who may not have the same access to some of the services. And it completely changed the entire dynamic.
MW: What sort of places were these happening?
DASKALAKIS: These are like pop-up vaccine sites. The thing that was really important was that it demonstrates that though we can give national guidance, public health is really a local show. It’s the way that our system is built. And so I think that, again, providing the guidance that the states need and good technical assistance to figure out how to do good distribution is important. But then it’s also important that we allow them the opportunity to know their own environment and do what they think is right.
With that said, their community also talks back to them, and just like we hear from the community, that iterative process changes things. And I saw that in practice in Atlanta, where the community said, “Whoa, wait a minute, this was not an equitable distribution.” And then the second round, I was like, “This is great. Completely different demographic, completely different dynamic.” And it’s just these little equity adjustments that you get from the knowledge of what you’re doing ends up being so critical.
MW: I think we’ve seen a little bit of that shift in D.C. By most accounts, it was all gay white men at that first round of doses, and I was part of the second round that D.C. let out, and when I went, it was very diverse.
DASKALAKIS: So that’s a twin of what happened in Atlanta. And again, it just sort of reminds you that you should lead with the equity consideration. It’s not, “Oh round two will do it.”
MW: “Oh, we need to do this now.” You needed to do it before.
DASKALAKIS: But we know that you need to do it, because it always goes that way. It is a consistent finding in everything that we do. And the thing that’s really interesting about gay, bisexual, other men who have sex with men, is that you’re never going to run out of shoulders. The shoulders are every color. Because when you look at the COVID-19 data from an international immunization survey, let’s say that it was like 95% overall of gay men had the COVID shot, like it was, 96% were white and then like 89% were Black. Those are approximate numbers, and a little bit higher among Latinos. Now, there’s a disparity there, right?
But in public health and in HIV, the disparities are usually like three times bigger. And so, for vaccines that people really want, I don’t think we’re going to have that same issue. It’s just making sure that there’s access. Because the willingness, the confidence is there. People are ready. It’s just making sure that the access is equitable.
MW: Last question, sort of generally interpreting the AIDS 2022 theme of “Re-engage and follow the science.” How do you interpret that? How do you and/or CDC interpret that into a concrete strategy?
DASKALAKIS: Testing. For HIV, the answer is testing, treatment, PrEP, and response. Our four pillars are science-based. And as we’re dealing with the new normal of COVID-19, I think that we’re in a really important position, where we’ve learned lessons that are good, some hard-learned, to really reinvigorate the work and focus on the science.
If you test people, it’s a gateway that opens the door to either treatment or prevention. If you treat people, viral suppression, U=U, they don’t transmit, which is a good side effect but really it means that they stay healthy, and their quality of life is good.
HIV-negative folks could benefit from prevention. You get them on PrEP, they don’t get HIV. And if you find a cluster of infections that are happening in the community, you can intervene on those, and get them the services which happen to be testing, treatment, and PrEP to make sure that they’re addressing the outbreak as well as preventing future outbreaks.
As Dr. Fauci said, we have the science. We know what the science is and what we need to do. Now it’s about the implementation. And having lived through two and a half years of pandemic, really getting on the other side and working with that new normal to reinvigorate the work that we do. So I think it’s a very resonant theme for the work that we’re doing in the U.S.
[wpforms id=”213051″]
[wpforms id=”213046″]
Support Metro Weekly’s Journalism
These are challenging times for news organizations. And yet it’s crucial we stay active and provide vital resources and information to both our local readers and the world. So won’t you please take a moment and consider supporting Metro Weekly with a membership? For as little as $5 a month, you can help ensure Metro Weekly magazine and MetroWeekly.com remain free, viable resources as we provide the best, most diverse, culturally-resonant LGBTQ coverage in both the D.C. region and around the world. Memberships come with exclusive perks and discounts, your own personal digital delivery of each week’s magazine (and an archive), access to our Member's Lounge when it launches this fall, and exclusive members-only items like Metro Weekly Membership Mugs and Tote Bags! Check out all our membership levels here and please join us today!






























You must be logged in to post a comment.